psychologist, trainer, consultant
Dr. Amy
Featuring Articles for HEALTH CARE PROVIDERS, EDUCATORS, AND PARENTS
Welcome to the Blog
Have a topic idea? Reach out to me at info@doctoramyllc.com with your ideas!
SUBSCRIBE TO THE NEWSLETTER
MEET DR. AMY
Learn more
Dr. Amy King, aka Dr. Amy, is a licensed psychologist who provides training, consultation, and education to medical providers and clinics. Among her specialties is working with professionals to help create resilient children, patients and thriving families, guiding them to heal their stress and trauma through connected relationships. Her experience includes serving as a statewide trainer for the Oregon Department of Human Services and subject matter expert to promote child wellness in pediatric settings on behalf of the Children's Health Alliance. Her current work is promoting resilience within primary care medical homes and through partnership and collaboration via her podcast, her membership, and speaking opportunities and trainings.
Educator friends, skip to the end of this newsletter and grab your spot for our free workshop this week! The rest of you, read on for a dose of compassion!! We’re carrying around a lot right now. When I explain the weight of what we carry during presentations, I use the “suitcase analogy.” As we enter into another […]

read now
If you’re a professional working with kids and families and want to do so in a trauma-informed way, in community with other like-minded professionals, we’ve got you covered. In May, we’re hosting TWO open houses in our ConnectEd Collabs for professionals and you can find your link to join us below! Does this sound familiar to you? If this […]

read now
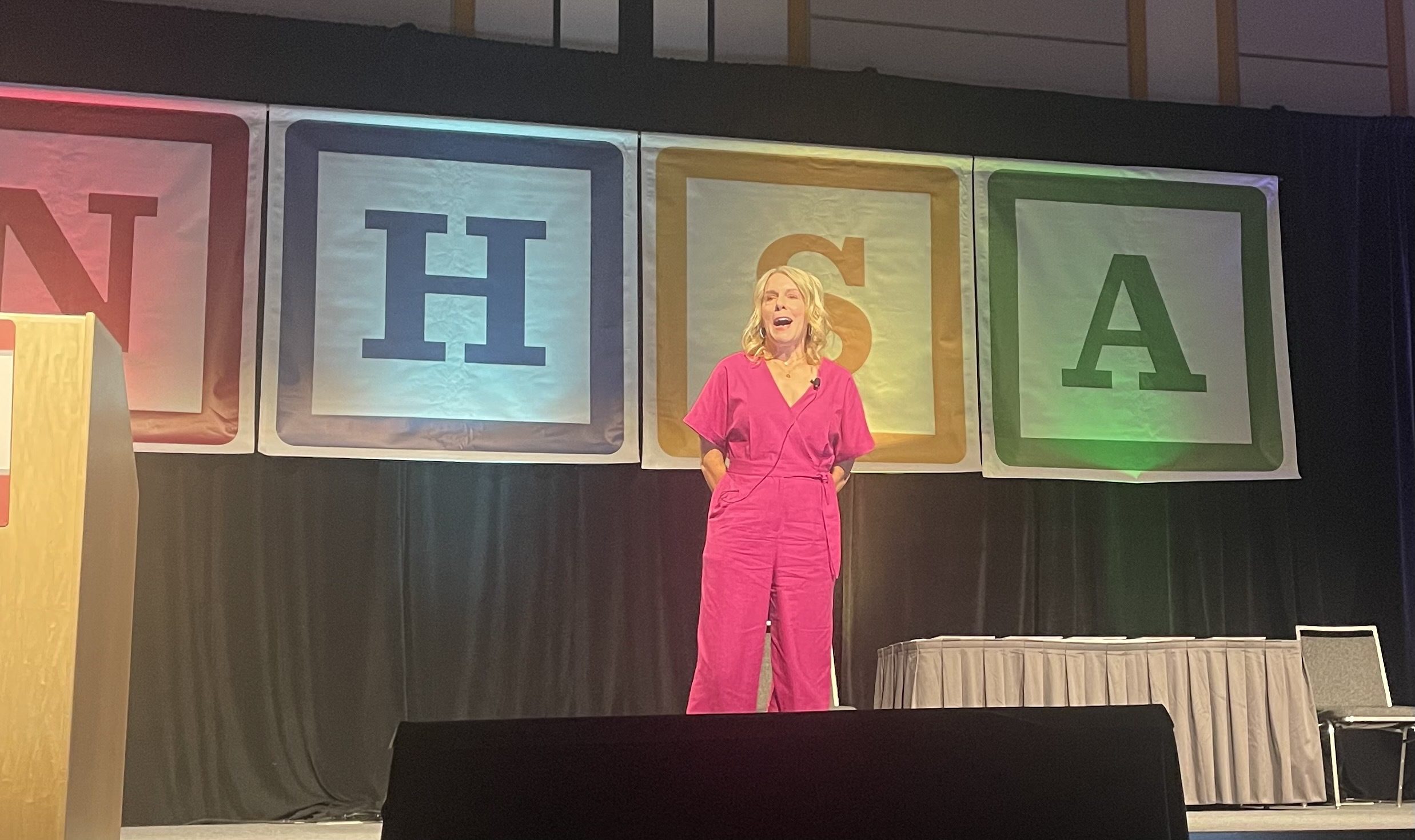
My team and I had an AMAZING TIME at the National Head Start Conference this week. I had the honor and privilege of presenting as their keynote speaker for the 51st Annual Conference in Portland. Hearts were inspired, souls were lifted! If you’re interested in inviting me to speak, reach out soon because our summer and fall dates are […]
read now
I’m returning from a fantastic weekend of business AND pleasure! Here’s a fun re-cap and a little insider scoop into my very busy past few months! I just spent the past 5 months working with a wonderful healthcare organization, a Federally Qualified Health Center (FQHC), on trauma-informed practices. It’s been inspiring, challenging, and soul-filling to […]

read now
This past week, our family vacationed in Hawaii. I’ve been taking my kids there since they were little and I’m sure it’s part of their core memories, as most family rituals become. We’re a friendly crew and as we waited on the beach we began chatting with another family. My children, at 17 & 19, […]

read now
If you’re paying attention to social media of late, there’s a book that’s getting a LOT of attention. It’s called Bad Therapy, written by Abigail Shrier. The basic summary is that children are being over-therapized without reason. She vilifies therapists, parenting experts and other school-based programs, often lumping these professionals together. She posits that well-intentioned […]
read now
I was recently scrolling through social media trying to find a picture of someone to share with a friend. I went to my friend’s account and realized she had deleted hundreds of photos from her social media account. When I asked about why those photos had been deleted, she said, “Oh, I’m not in that […]

read now
Friends, I started my private practice in 2003. I was a baby psychologist, just licensed. I set up my sweet little office in Clackamas Oregon and put out my shingle. You came. You trusted me with your stories, your children, your lives, and your hearts. Between 2003 and 2015 we grew together. Clients came and went […]

read now
Friends, I’m giving you a little sneak peek into my upbringing today. It’s certainly an insight into how I operate. But, it’s also a GREAT opportunity to differentiate grit & perseverance from resilience. On Super Bowl Sunday, we hosted a small gathering at our home. Just a few families gathered to watch the Chiefs & 49ers, […]

read now
Friends, My podcast has made its way to 80 episodes! I’m so happy with the stories that are out in the world because of this brave endeavor. Stories of hope, healing, and connection wrapped up in trauma-responsive love – I’m proud of this work that my team and I have created. But for now, I’m […]
read now